Glaucoma is the name given to a group of eye conditions in which the optic nerve at the back of the eye is slowly damaged.
What is Glaucoma?
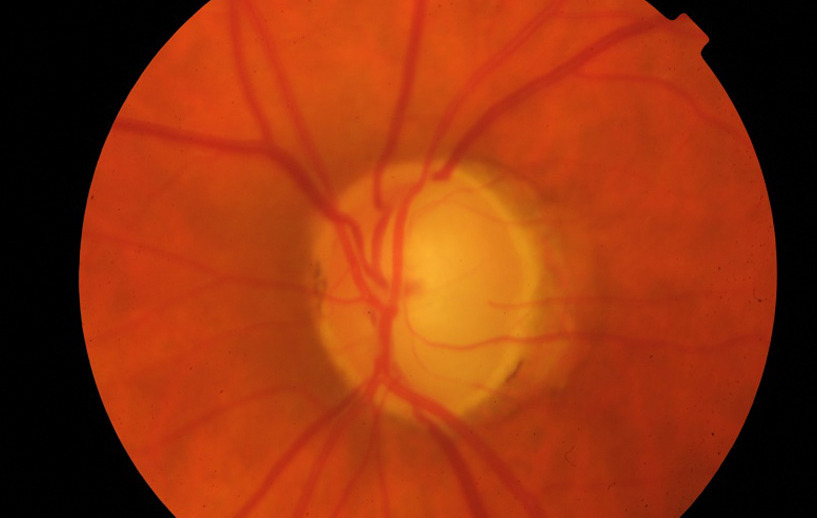
Glaucoma is the name given to a group of eye conditions in which the optic nerve at the back of the eye is slowly damaged. The diagnosis of glaucoma is made when your optometrist or ophthalmologist notices a particular type of damage in the optic nerve known as “cupping.” This diagnostic finding can occur with or without increased pressure inside the eye.
Intraocular Pressure
A normal intraocular pressure (IOP) ranges between 10 and 21 mmHg (millimeters of mercury, a measurement of pressure). While it is more likely that you will have or develop glaucoma if your eye pressures are high, many people with high eye pressures never develop glaucoma. Furthermore, some people with glaucoma never have high eye pressures. Glaucoma with eye pressure in the normal range is known as “normal-tension glaucoma.”
What will I notice?
Chronic (primary open-angle) glaucoma is the most common type. It has no noticeable symptoms until eye sight is severely damaged.
Damage progresses very slowly and destroys vision gradually, starting with the side vision. One eye covers for the other, and the person remains unaware of any problem until a majority of nerve fibres have been damaged, and a large part of vision has been destroyed. This damage is irreversible. It is progressive and usually relentless. Treatment cannot recover what has been lost. But it can arrest, or at least, slow down the damage process. That is why it is so important to detect the problem as early as possible, to be able to start treatment with as little damage to the vision as possible.
Establishing a diagnosis
To confirm the diagnosis, or to assess your risk of glaucoma, a number of tests are carried out in our clinic. These include:
- Intraocular pressure measurement
- Pachymetry – corneal thickness measurement. This can affect the interpretation of the IOP measurement
- Computerised visual field test – this assesses your peripheral, or side vision. Glaucoma tends to affect the peripheral before the central vision. Patients tend not to notice this peripheral visual deterioration until it is severe. This test takes about 5 minutes per eye, and can be mentally challenging, especially if you have not done it before. It is not uncommon to have to repeat this test at another visit to establish a reliable and consistent result
- OCT scan – this machine assesses the health of the optic nerve. The scan measures the thickness of the nerve fibres in minute detail. It is also useful in assessing if the optic nerve damage changes over time
- Gonioscopy – your ophthalmologist will place a small lens on the surface of your eye after a drop of anaesthetic is used. This takes a few seconds and does not hurt. This is to assess the drainage area in your eye, and to establish the type of glaucoma you may have
- Dilated eye exam – after you pupils are dilated (opened) with an eye drop, your ophthalmologist will look into the back of your eye to assess your optic nerve for “cupping”.
Treatment
The goal of treatment is to lower the eye pressure to minimise the risk of further damage to the optic nerve, and therefore, your vision. Lowering eye pressure can be accomplished using eye drops, laser, or surgery. Treatment needs to be carried out for life. Glaucoma can be controlled, but there is currently no cure. Glaucoma treatment will not improve your vision.
When eye drops are chosen, it is important that you instill them appropriately and regularly. Some of the drops need only be used once daily while some require twice or three times a day dosing. Like any medication, eye drops can potentially have side effects, and these may not be limited to the eye. For example, timolol eye drops can cause breathing problems in asthmatic patients.
The laser to lower eye pressure is called Selective Laser Trabeculoplasty. This has been shown to be as effective a first treatment option as eye drops. This is a simple, mostly painless, quick procedure that can control eye pressure for a period of up to 5 years in some patients.
Many surgeries are available and newer ones are being constantly developed and evaluated. Most of these are reserved for patients with advanced glaucoma, not adequately controlled with drops and laser.
The choice of treatment depends on many factors which are unique to each patient and should be discussed with your ophthalmologist. If you start with eye drops, but are having difficulty putting them in, forget frequently, or are having side effects, tell your ophthalmologist, and other options can be discussed.
Monitoring
Once a diagnosis and treatment plan is established, the eye pressure and optic nerve need to be monitored. If all is stable, you generally need eye pressure checks every 6 months. OCT scans and visual field tests should be repeated at least yearly. If there is evidence of progressive damage, or in advanced disease, these checks may need to be more frequent.
Your optometrist can also help in monitoring glaucoma. Your local doctor (GP) can prescribe your glaucoma drops, but will not have the equipment to assess your eye pressure.
Will I go blind?
When faced with a new diagnosis of glaucoma there is one question that is foremost in every patient’s mind: “Will I go blind?”
Fortunately for most patients the answer is no. Blindness does occur from glaucoma but it is a relatively rare occurrence. Blindness occurs in about 5% of glaucoma patients, and usually occurs when the diagnosis is made late, when the disease is already advanced. Sight impairment is more common and occurs in around 10% of patients.
Loss of vision can occur even with the best treatment. Despite that sobering fact, correct treatment and follow-up will stabilise the vast majority of patients with glaucoma. A major factor in the treatment of your glaucoma is you. By correctly using your eye drops and being consistent in their use, a favorable outcome will be more likely.
Further information
We have brochures available in our clinic on glaucoma and selective laser trabeculoplasty.
Glaucoma Australia website: www.glaucoma.org.au
If you are having trouble putting drops in your eyes, there is an instructional video on the Glaucoma Australia website. Alternatively, there are special devices to help with eye drop installation. Please discuss with our staff, or your pharmacist.