Case Studies: Left Branch Retinal Vein Occlusion
A 40 year old patient presented with sudden onset of painless vision loss from his left eye. There were no associated ocular symptoms and he was systemically well, though moderately over weight.
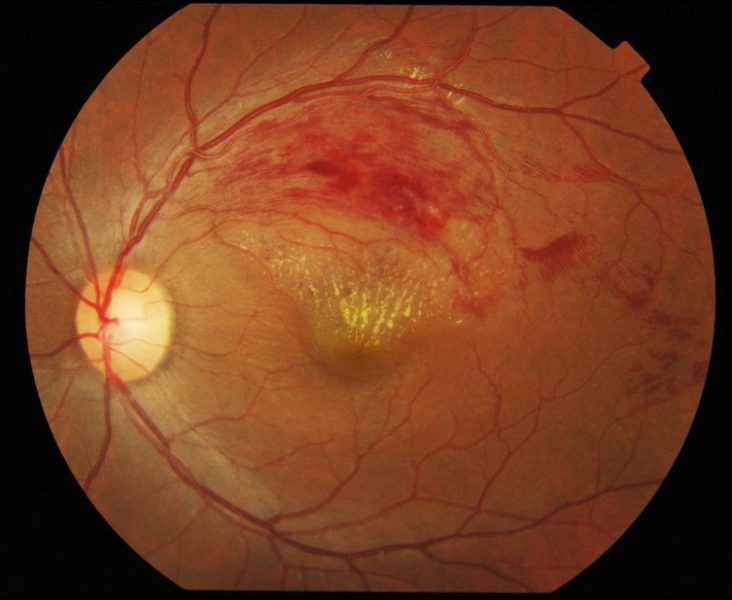
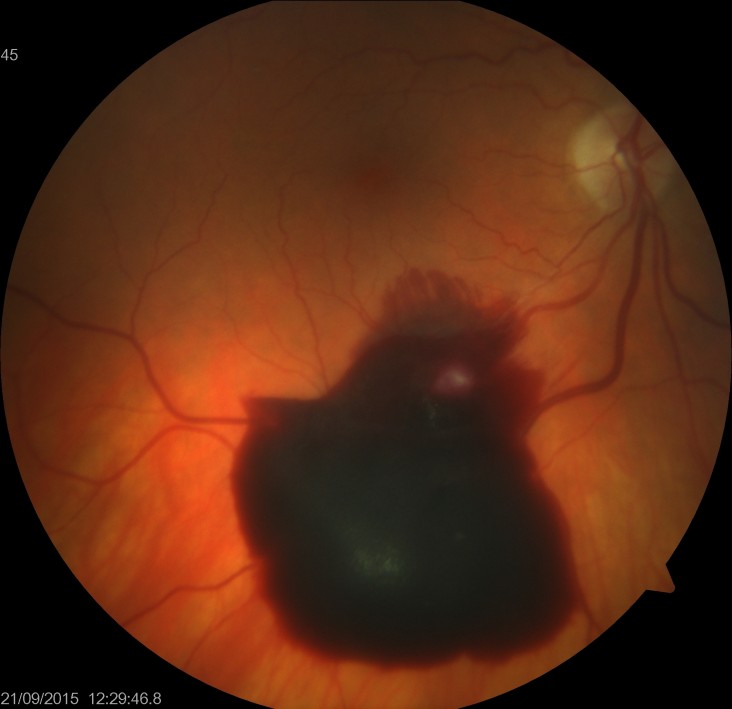
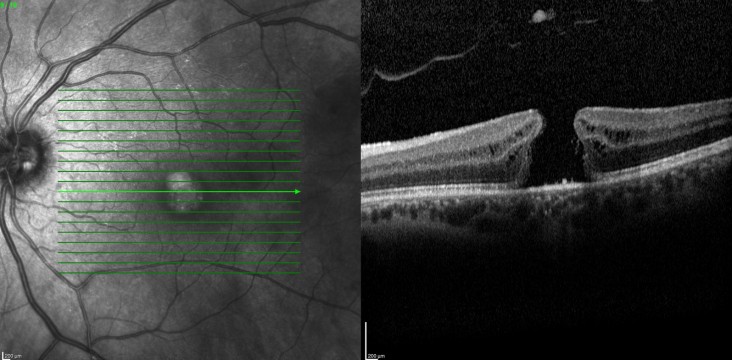
On examination his corrected acuities were right 6/6 and left 6/90. His intraocular pressures were normal. His anterior segments were unremarkable with clear ocular media and no rubeosis. Dilated fundus examination on the right was essentially unremarkable and on the left there were retinal haemorrhages and cotton-wool spots, along the superotemporal arcade, consistent with a branch retinal vein occlusion. On OCT scanning, he had significant associated macular oedema (see figure 1).
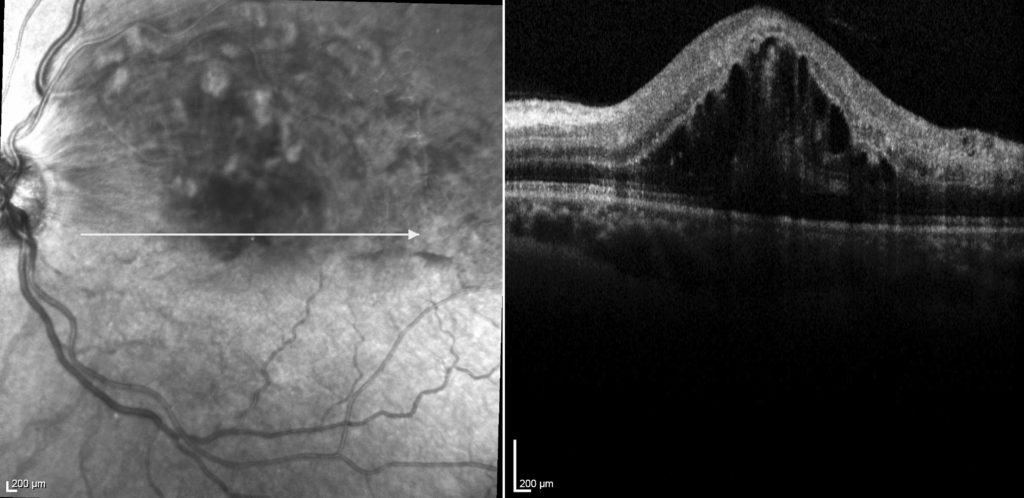
FIG 1
The patient was diagnosed with a left branch retinal vein occlusion. The most common cause underlying cause is atherosclerotic disease, associated with systemic hypertension. However, given this patient was only 40 years of age, obstructive sleep apnoea and pro-coagulant diseases need to be ruled out.
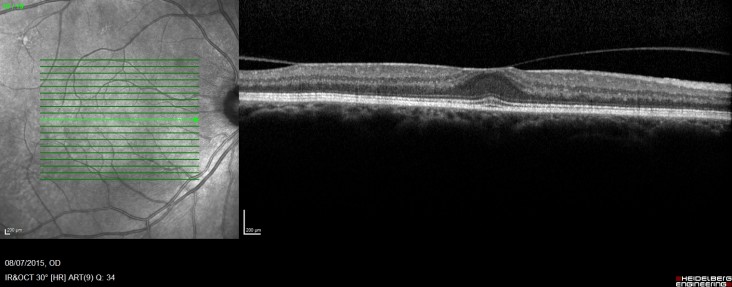
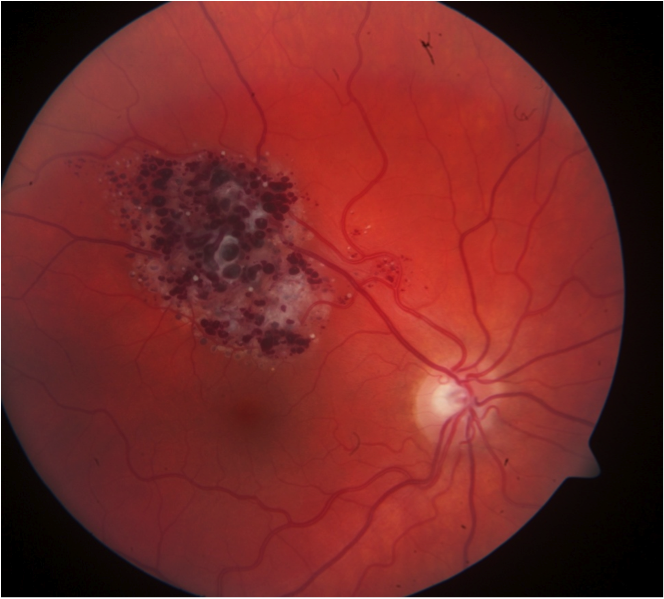
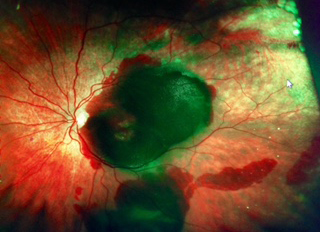
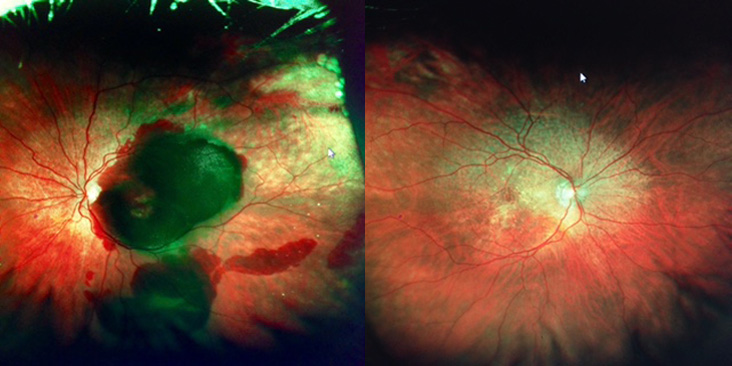
Treatment of intravitreal Lucentis injection therapy was instituted, and four weeks after the first injection his vision returned to 6/9 and his macular oedema dramatically improved, as seen in figure 2 below.
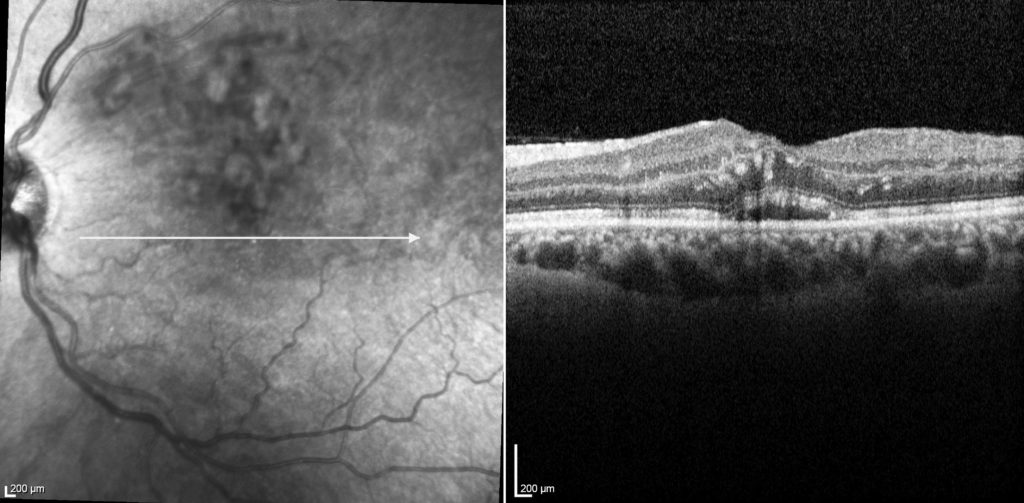
FIG 2